DOAC Switch Timing Calculator
INR Guidance for Switching
Enter your latest INR value to determine safe timing for switching from warfarin to a DOAC. Always confirm kidney function before proceeding.
Switching from warfarin to a direct oral anticoagulant (DOAC) can simplify your life-no more weekly blood tests, fewer food restrictions, and less worry about drug interactions. But if done wrong, it can also put you at risk for stroke, dangerous bleeding, or worse. This isn’t just a prescription change. It’s a medical transition that needs precision, timing, and careful planning.
Why Switch at All?
Warfarin has been the go-to blood thinner for over 70 years. But it’s finicky. You need regular INR checks-often every 1-4 weeks-to make sure your blood isn’t too thin or too thick. Even small changes in diet, other meds, or illness can throw off your dose. Many people find this exhausting. DOACs like rivaroxaban, apixaban, dabigatran, and edoxaban don’t need that kind of monitoring. They work more predictably. Studies show they’re just as good at preventing strokes in people with atrial fibrillation-and better at reducing the risk of bleeding in the brain. For most patients, that’s a win.When You Shouldn’t Switch
Not everyone is a candidate. If you have a mechanical heart valve, switching to a DOAC is dangerous and not recommended. DOACs don’t work well in these cases, and the risk of clotting on the valve is high. Same goes if you’re pregnant or breastfeeding. DOACs can cross the placenta or enter breast milk, and we don’t have enough safety data to recommend them. Severe kidney problems also rule out most DOACs. If your creatinine clearance is below 15-30 mL/min (depending on the drug), your body can’t clear the medication properly. That raises bleeding risk. Liver disease, especially Child-Pugh Class C, is another red flag. Your liver helps break down these drugs. If it’s failing, levels can build up dangerously. Even body weight matters. If you weigh less than 60 kg or more than 150 kg, you were mostly left out of the original clinical trials. That means we don’t know exactly how safe or effective the standard doses are for you. Your doctor may need to adjust or choose carefully.The Critical Timing: INR Is Your Guide
This is where mistakes happen. You can’t just stop warfarin one day and start a DOAC the next. You have to wait until the warfarin effect wears off-but not too long, or you’re unprotected. The key is your latest INR number:- If your INR is ≤2.0: Start the DOAC right away.
- If your INR is 2.0-2.5: Start the DOAC the same day or the next day.
- If your INR is 2.5-3.0: Wait 1-3 days, then recheck your INR before switching.
- If your INR is ≥3.0: Don’t switch yet. Wait 3-5 days and retest.
Which DOAC to Choose? It Depends on You
Not all DOACs are the same. Here’s a quick breakdown:| Drug | Max INR to Start | Renal Clearance Needed | Special Notes |
|---|---|---|---|
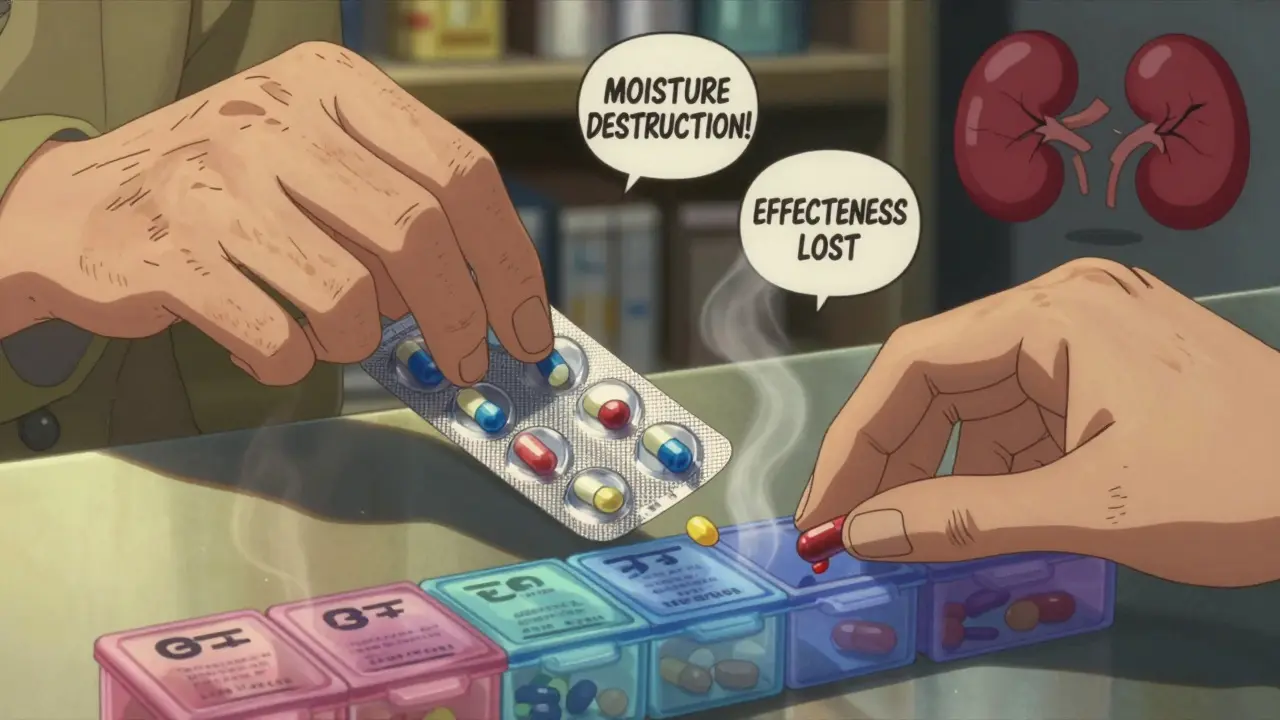
| Dabigatran | ≤2.0 | CrCl ≥30 mL/min | Keep in original bottle-moisture ruins it. Can’t be put in pill boxes. |
| Rivaroxaban | ≤3.0 | CrCl ≥15 mL/min | Take with food for best absorption. |
| Apixaban | ≤2.0 | CrCl ≥15 mL/min | Lower bleeding risk than others. Often preferred in older adults. |
| Edoxaban | ≤2.5 | CrCl ≥15 mL/min | Dose adjusted if weight ≤60 kg or if taking verapamil. |
Side Effects You Might Notice
DOACs are generally safer than warfarin-but they still carry risks. The biggest concern during the switch is bleeding. You might notice:- Bright red blood in stool or dark, tarry stools
- Unusual bruising or swelling
- Bleeding gums when brushing teeth
- Headaches, dizziness, or weakness (could signal brain bleeding)
- Red or pink urine
What Happens Before, During, and After the Switch?
A smooth transition follows a clear plan:- Check your recent bloodwork-creatinine, liver function, full blood count-within the last 6 months.
- Calculate your creatinine clearance using the Cockcroft-Gault formula. This tells your doctor how well your kidneys are working.
- Get your INR tested the day before or the day of the switch.
- Based on that INR, your doctor decides exactly when to stop warfarin and start the DOAC.
- Get clear written instructions: what to take, when, and what to watch for.
- Ask for an anticoagulant alert card and patient information leaflet. Keep it with you.
- Follow up with your pharmacist. Many offer a New Medicine Service to check how you’re doing after 2 weeks.
Special Situations: Surgery, Falls, and Older Adults
If you’re scheduled for surgery or a dental procedure, your DOAC needs to be paused. But how long? It depends on your kidney function and the procedure’s bleeding risk:- For a low-risk procedure (like a tooth extraction) and normal kidney function (CrCl >90 mL/min): Hold dabigatran for 24-36 hours.
- For a high-risk procedure (like hip replacement) and moderate kidney impairment (CrCl 30-50 mL/min): Hold dabigatran for 96-108 hours.
What About Cost?
In the UK, DOACs are generally available on the NHS with no extra cost to patients. But in places like the US, warfarin costs $10-30 a month, while DOACs can run $500-700. That’s why some doctors hesitate to switch unless the patient has clear benefits-like trouble with INR control or a history of bleeding. But cost isn’t the whole picture. If you’ve had a brain bleed on warfarin, switching to a DOAC might save your life. If you’ve been struggling with weekly blood draws, the convenience alone improves your quality of life and adherence.What If You Switch Back?
Sometimes, switching back to warfarin is necessary-maybe because of kidney failure, cost, or a major bleed. But this is trickier than switching to a DOAC. You can’t just start warfarin and expect it to work right away. You usually need to overlap it with a fast-acting shot (like heparin) until your INR reaches the target range. That’s why it’s best to avoid switching back unless absolutely needed.Final Advice: Don’t Rush, Don’t Guess
This isn’t a decision you should make alone. Only doctors trained in anticoagulation management should handle the switch. Pharmacists can help with dosing and education, but the decision must come from someone who understands the full picture. If you’re thinking about switching, ask:- What’s my current INR?
- What’s my creatinine clearance?
- Do I have any kidney or liver problems?
- Am I on any other meds that might interact?
- What’s the plan if I miss a dose or have surgery?
Can I switch from warfarin to a DOAC on my own?
No. Switching requires precise timing based on your INR and kidney function. Only clinicians trained in anticoagulation management should make this decision. Doing it without proper testing can lead to stroke or dangerous bleeding.
Which DOAC has the lowest risk of bleeding?
Apixaban has consistently shown the lowest risk of major bleeding in clinical trials, especially in older adults and those with kidney issues. It’s often the preferred choice when bleeding risk is a concern.
Do I still need blood tests after switching to a DOAC?
You won’t need INR tests anymore. But you should still get kidney function checked every 6-12 months, especially if you’re over 75 or have other health conditions. Liver tests may also be checked occasionally.
Can I take DOACs with food?
It depends. Rivaroxaban must be taken with food to be absorbed properly. Dabigatran, apixaban, and edoxaban can be taken with or without food. Always follow your doctor’s instructions.
What if I miss a dose of my DOAC?
If you miss a dose and remember within 6 hours of your usual time, take it right away. If it’s been longer, skip the missed dose and take your next one at the regular time. Never double up. Missing doses increases your risk of clotting.
Are DOACs safe during pregnancy?
No. DOACs can cross the placenta and harm the developing baby. If you’re pregnant or planning to become pregnant, warfarin may be used under strict supervision, or you may need injections like heparin instead. Always talk to your doctor before stopping or starting any blood thinner during pregnancy.
Can I use a pill organizer for my DOAC?
You can use one for rivaroxaban, apixaban, and edoxaban. But dabigatran is moisture-sensitive and must stay in its original blister pack. Putting it in a pill organizer can reduce its effectiveness.


henry mateo
December 29, 2025 AT 20:54just switched to apixaban last month and holy crap it’s been a game changer. no more weekly blood draws, i actually remember to take it because it’s just… easier. still scared of bleeding but my doc gave me that alert card and i carry it everywhere like a security blanket 🙏
Aayush Khandelwal
December 31, 2025 AT 03:59the INR thresholds for switching are non-negotiable. if you skip the lab test and just wing it, you’re playing russian roulette with your cerebral vasculature. DOACs aren’t magic-they’re pharmacokinetic tightropes. one miscalculation and you’re in ICU with a subdural hematoma. respect the algorithm.
Glendon Cone
January 1, 2026 AT 03:27apixaban for the win 🏆 seriously, if you’re over 70 or have kidneys that don’t work like they used to, this is the one. my grandma’s on it, no bruising, no drama. she even forgets to take it sometimes and lives to tell about it 😅
srishti Jain
January 3, 2026 AT 01:56so you’re telling me i can’t use my pill organizer for dabigatran? lol. guess i’ll just throw it in the drawer with my expired coupons.
Colin L
January 3, 2026 AT 16:59i’ve been on warfarin for 12 years and i’m not switching. you think DOACs are safer? tell that to the guy who bled out in the ER because his nephrologist didn’t check his CrCl. people die from this stuff every day because doctors treat it like a menu choice. it’s not. it’s a minefield wrapped in a marketing brochure.
Nadia Spira
January 3, 2026 AT 18:35apixaban is the "safe" choice? sure. until you realize the clinical trials excluded 80% of real-world patients. elderly, obese, diabetic, on polypharmacy? yeah, they didn’t study those people. so you’re just a data point in a pharma-funded fantasy. congrats on your placebo effect.
Hayley Ash
January 4, 2026 AT 17:56so let me get this straight-i can’t switch if i’m under 60kg or over 150kg because they didn’t study us? wow. so if i’m fat or tiny i just get to die on warfarin? thanks for the clarity
Sandeep Mishra
January 5, 2026 AT 13:12to anyone thinking about switching: talk to your pharmacist. they’re the unsung heroes here. they’ll catch interactions your doctor missed, remind you about food with rivaroxaban, and actually explain why you can’t put dabigatran in a pill organizer. don’t underestimate them. i used to think they were just cashiers. now i call them my anticoagulation angels.
Kelly Gerrard
January 6, 2026 AT 07:45switching to a DOAC requires disciplined adherence. missing a dose increases stroke risk by 200%. this is not a casual medication. if you cannot commit to taking it at the same time every day, warfarin remains the more reliable option despite its burdens.
Kunal Karakoti
January 8, 2026 AT 07:27it’s funny how we treat anticoagulation like a technical problem to be optimized. but it’s really about trust. trust in your body’s fragility. trust in the precision of science. trust that your doctor isn’t rushing you. and trust that you won’t forget tomorrow’s pill. the real switch isn’t from warfarin to dabigatran-it’s from passive compliance to active stewardship of your own survival.
Cheyenne Sims
January 9, 2026 AT 00:13the notion that DOACs are "better" is a dangerous myth propagated by pharmaceutical lobbying. warfarin has decades of real-world evidence. DOACs have glossy trials funded by companies that profit from their high cost. in America, this isn’t medicine-it’s capitalism disguised as innovation.
Henry Ward
January 9, 2026 AT 14:42you think this is complicated? try being the family member who has to clean up the blood after your mom falls and bleeds internally because she skipped her dose. DOACs sound nice until you’re wiping up a puddle of red on your kitchen floor at 3am. no one talks about that part.
Shae Chapman
January 11, 2026 AT 13:44i switched last year and cried the first time i didn’t have to go to the lab. no more pinpricks, no more waiting for results, no more feeling like a lab rat. i feel like i got my life back. apixaban is my new best friend 💕
Joseph Corry
January 13, 2026 AT 03:55the entire narrative around DOACs is a neoliberal fantasy. you’re not "freed" from blood tests-you’re just handed a more expensive, irreversible chemical leash. the system doesn’t care if you live or die. it cares if you keep buying. don’t be fooled by convenience. it’s just a more stylish cage.
kelly tracy
January 13, 2026 AT 06:03my dad switched to rivaroxaban and had a GI bleed three weeks later. they didn’t even check his liver. now he’s on warfarin again and they say "oh well, you were too high risk." so why did they switch him in the first place? this system is broken and everyone knows it.