When you take a new medication, your body might react in ways you didn’t expect. Maybe you feel nauseous after taking your antibiotic. Or your skin breaks out in hives after your first dose of ibuprofen. You might assume it’s an allergy - and many people do. But here’s the truth: side effects, allergic reactions, and intolerance are not the same thing. Confusing them can lead to unnecessary fear, wrong treatments, and even dangerous health choices.
What’s Really Happening When Your Body Reacts?
Not every bad reaction to a drug means you’re allergic. In fact, only about 5-10% of people who say they have a drug allergy actually do. The rest are experiencing side effects or intolerance - two very different things. A side effect is a known, predictable reaction that comes from how the drug works in your body. For example, NSAIDs like ibuprofen block inflammation, but they also irritate the stomach lining. That’s why 25-30% of people get nausea or stomach upset. It’s not random. It’s built into the drug’s chemistry. These reactions are dose-dependent - the more you take, the worse it gets. And often, they fade over time. If you start metformin for diabetes and get diarrhea, your body usually adjusts within a few weeks. Your doctor might even tell you to take it with food. That’s managing a side effect - not avoiding the drug forever. An allergic reaction is your immune system going into overdrive. It mistakes the drug for a threat and launches an attack. This isn’t about dosage. Even a tiny amount can trigger it. Symptoms come fast: hives, swelling of the lips or tongue, trouble breathing, a sudden drop in blood pressure. These are signs of anaphylaxis - a medical emergency. If you’ve ever needed epinephrine after taking a drug, that’s a true allergy. It’s not something you grow out of. And it’s not something you can test at home. Only a specialist can confirm it with skin tests or controlled challenges. Then there’s intolerance. This one’s tricky because it’s not clearly defined. It’s when your body reacts badly to a drug at normal doses - but not because of your immune system. Think of it like being extra sensitive to caffeine. One cup gives someone else a little buzz. You get a racing heart and anxiety. Same drug. Different body. A classic example is aspirin-exacerbated respiratory disease. About 7% of people with asthma get wheezing or nasal polyps after taking NSAIDs like aspirin or ibuprofen. But they can often take celecoxib, a different kind of NSAID, just fine. This isn’t allergy. It’s pharmacological intolerance - your body’s metabolism or receptors just don’t handle it well.How to Spot the Difference
Here’s a simple way to tell them apart:- Timing: Allergies hit fast - usually within minutes to an hour. Side effects and intolerances can show up anytime, even after days of use.
- Symptoms: Hives, swelling, wheezing, low blood pressure? That’s allergy. Nausea, dizziness, headache? That’s likely a side effect. If you get breathing trouble every time you take NSAIDs but not other drugs, that’s intolerance.
- Repetition: If you took the drug before and had no problem, then suddenly got hives? That’s probably an allergy. If you’ve always felt sick after taking the same pill? That’s likely a side effect or intolerance.
- Response to dose: Cut the dose in half and the reaction disappears? Probably a side effect. Still react even with a tiny amount? That’s allergy.
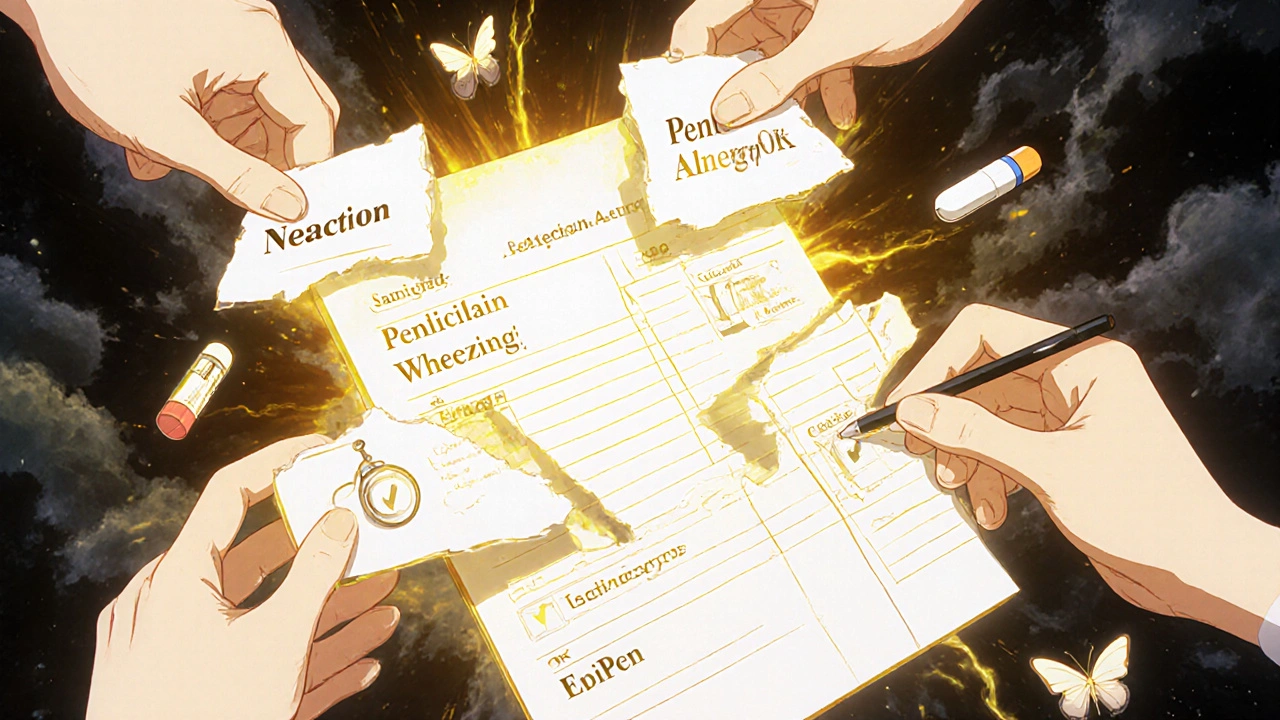
One of the most common mistakes? Labeling diarrhea from amoxicillin as a penicillin allergy. That’s a side effect - not an immune response. Yet millions of people carry that label in their medical records. And it has real consequences.
Why It Matters: The Hidden Cost of Mislabeling
If you say you’re allergic to penicillin - even if you’re not - doctors will avoid it. They’ll use stronger, broader antibiotics instead. That’s a problem. The CDC says only 1% of people who say they’re allergic to penicillin actually are. But 10% of Americans claim the allergy. That mismatch leads to:- 30% higher risk of C. diff infection
- 50% higher risk of MRSA infection
- Longer hospital stays - by an average of 1.2 days
- $2,500 more in annual healthcare costs per person
And it’s not just penicillin. People avoid sulfa drugs because they got a rash once - but that rash might’ve been a viral infection, not the drug. They avoid NSAIDs because they got a headache - not realizing that’s a common side effect of many painkillers.
One patient I read about avoided all antibiotics for 15 years after a single episode of nausea with amoxicillin. She ended up with a severe lung infection because her doctors had to use second-line drugs. After allergy testing, she found out she was never allergic. She’s taken amoxicillin eight times since - no issues.
What You Should Do
If you’ve ever had a reaction to a drug, don’t just assume it’s an allergy. Ask yourself:- Did I have hives, swelling, or trouble breathing?
- Did it happen within an hour of taking the drug?
- Did I need epinephrine or an ER visit?
If the answer is yes - see an allergist. Get tested. Don’t live with a label that might be wrong.
If the reaction was nausea, dizziness, or a mild rash that didn’t involve breathing or swelling - that’s probably not an allergy. Talk to your doctor. Ask: "Is this a side effect? Can we adjust the dose or timing?"
And if you react badly to multiple NSAIDs but not others? That’s likely intolerance. Your doctor can help you find alternatives that work for your body.
What Doctors Are Doing About It
Hospitals across the U.S. are changing how they handle drug reactions. The SHIELD study, which covered 127 hospitals, showed that when allergists were brought in to review allergy labels, inappropriate avoidance dropped by 40%. Penicillin testing programs cut broad-spectrum antibiotic use by 35%. New tools are helping too. Electronic health records now pop up warnings: "Is this really an allergy?" They ask for details - timing, symptoms, treatment - before letting a provider mark it as an allergy. The FDA now requires drug labels to clearly separate allergy risks from side effects. And in 2023, the NIH funded a new point-of-care test for penicillin allergy that gives results in 15 minutes instead of three hours. Soon, your GP might be able to rule out an allergy during your visit.Don’t Let a Misunderstanding Limit Your Care
Medications save lives. But they only work if you can take them safely. If you’ve ever said, "I’m allergic to this," but you’re not sure why - it’s time to find out. You might be avoiding a drug you could safely use. Or you might be using something riskier because you think you have no other choice. The truth is simple: not every bad reaction is an allergy. And not every allergy is what you think it is. Getting it right isn’t just about comfort - it’s about safety, effectiveness, and your long-term health.Can I outgrow a drug allergy?
Unlike some food allergies, true drug allergies rarely go away on their own. If you had a severe allergic reaction - like anaphylaxis - to penicillin or sulfa drugs, you likely won’t outgrow it. But many people are mislabeled. Up to 90% of people who think they’re allergic to penicillin turn out to be fine after proper testing. That’s not outgrowing - it’s correcting a mistake.
Is a rash always a sign of an allergy?
No. Many rashes from medications are not allergic. A mild, flat, pink rash that appears days after starting a drug - especially antibiotics like amoxicillin - is often a viral rash, not a drug allergy. True allergic rashes (like hives) are raised, itchy, and appear quickly - usually within hours. If the rash is accompanied by fever, blistering, or peeling skin, it could be a serious condition like DRESS syndrome, which requires immediate medical attention.
Can I take a similar drug if I’m allergic to one?
Sometimes, yes - but only under supervision. For example, if you’re allergic to one NSAID like ibuprofen, you might tolerate celecoxib, which works differently. But if you had a true IgE-mediated allergy to penicillin, you should avoid all penicillin-class drugs (like amoxicillin) unless tested. Cross-reactivity varies by drug class. Always talk to an allergist before trying a similar medication.
What should I do if I think I had an allergic reaction?
If you had trouble breathing, swelling of the face or throat, or felt like you were going to pass out - seek emergency care immediately. After that, ask for a referral to an allergist. Don’t wait. Bring your medication list and write down exactly what happened: when you took it, what symptoms you had, how long they lasted, and what treatment you received. That information helps them decide if it was a true allergy.
Can I test for drug intolerance at home?
No. Drug intolerance can’t be tested with a blood or skin test like allergies can. It’s diagnosed by process of elimination - your doctor will review your history, symptoms, and possibly try a different drug in the same class to see how you react. Never try to test this yourself. Even a mild intolerance can turn dangerous if you push through symptoms.
Why do some people get side effects and others don’t?
Genetics, age, liver or kidney function, and other medications you’re taking all play a role. For example, 7% of Caucasians have a gene variation (CYP2D6) that makes them process codeine too quickly, turning it into morphine faster than normal. That’s why they get vomiting or drowsiness at normal doses - it’s not an allergy, it’s a metabolic quirk. Your body’s unique chemistry determines how you respond.


Christopher Robinson
November 19, 2025 AT 16:00Wow, this is one of the clearest breakdowns of drug reactions I’ve ever read. I used to think any rash meant "allergy" until I got a mild one after amoxicillin and later found out it was just a viral rash. So many people are unnecessarily avoiding life-saving meds because of confusion. Thanks for putting this out there.
harenee hanapi
November 21, 2025 AT 12:38Okay but can we talk about how EVERYONE just labels everything an allergy? I had a friend who swore she was allergic to ibuprofen because she got a headache once. Headache. Not hives. Not swelling. Just a headache. And now she takes Tylenol for everything even though it gives her liver issues. I swear, people treat meds like haunted objects. Like if it made you feel weird once, it’s cursed forever. 😭
James Ó Nuanáin
November 22, 2025 AT 07:25As a British physician with over two decades in clinical practice, I must commend the precision of this exposition. The conflation of pharmacological intolerance with IgE-mediated hypersensitivity is not merely a misnomer-it is a systemic failure of public health literacy. In the NHS, we have witnessed a 47% increase in inappropriate antibiotic prescriptions directly attributable to erroneous allergy labeling. This is not anecdotal. It is epidemiological. The SHIELD study findings corroborate what we see daily: misclassification begets morbidity. We must institutionalize allergist-led reviews at the point of prescription. Anything less is negligent.
Nick Lesieur
November 23, 2025 AT 13:35sooo... if i get dizzy after taking a pill, i'm not allergic? but if i get dizzy after eating a sandwich, i'm allergic to bread? lol. this whole thing feels like doctors trying to make us feel dumb for being scared of medicine. also, why do i have to go to an allergist to prove i'm not allergic? can't we just... not take the drug? 😴
river weiss
November 24, 2025 AT 10:35This is an essential public health resource. The statistics on C. diff and MRSA risks alone should compel every primary care provider to implement structured allergy clarification protocols. I’ve seen patients avoid penicillin for 20+ years based on a childhood rash that was likely viral. One formal skin test changed their entire treatment trajectory. Please share this with your doctors. And if you’ve ever been told you’re "allergic" to a drug-ask: "Was it anaphylaxis? Was it within an hour? Did I need epinephrine?" If the answer is no, it’s probably not an allergy. Don’t carry a label that could cost you your life.
Brian Rono
November 26, 2025 AT 07:07Let’s be real-this isn’t about medicine. It’s about control. Doctors want you to trust them blindly, so they rebrand side effects as "normal" and allergic reactions as "rare." Meanwhile, you’re the one who’s got to live with the nausea, the brain fog, the anxiety after every pill. They’ll say "it’s not an allergy" while you’re shaking in the bathroom wondering if this is the time your body finally says "enough." Maybe the real problem isn’t your misunderstanding-it’s their dismissal.
seamus moginie
November 27, 2025 AT 15:51Brilliant breakdown. I had a patient once who refused all NSAIDs because she got a stomach ache after taking aspirin in her 20s. Turns out she had a GI sensitivity-not an allergy. We switched her to celecoxib and she’s been pain-free for 5 years. The real tragedy? She almost missed her daughter’s wedding because she was afraid to take any painkiller. Knowledge saves lives. And weddings.
Dana Dolan
November 28, 2025 AT 10:52thank you for this. i used to think i was allergic to penicillin bc i got a rash when i was 8. turns out it was a virus. got tested last year and now i’ve taken it 3x. no probs. why do we let childhood stuff stick like this? 🙃
Zac Gray
November 30, 2025 AT 08:27Okay, I’ll admit-I used to be the guy who just Google-searched "allergic to amoxicillin" and then self-diagnosed. But after reading this? I went to my doctor. Got tested. Turned out I wasn’t allergic-I just had a weird GI reaction that went away after taking it with food. Now I’m not the guy who makes the ER staff sigh when they see "penicillin allergy" in my chart. Honestly? This post saved me from years of unnecessary meds and higher bills. If you think you’re allergic but it’s just nausea or a rash that didn’t swell or breathe? Go get checked. It’s not a hassle. It’s a gift to your future self.
Steve and Charlie Maidment
December 1, 2025 AT 17:15so like... if i get sleepy after taking a drug, that's just a side effect? but if i get sleepy after eating a banana, that's a food allergy? why does this feel like semantics? also, why do i have to trust a doctor's guess about whether it's 'intolerance' or 'allergy'? what if i just... don't want to take it? isn't my body's warning enough? 🤷♂️
Andrew Baggley
December 2, 2025 AT 14:42Let me just say this: if you’ve ever been told you’re allergic to a drug and you’ve never had a true emergency reaction-stop assuming. Get tested. It’s not about being brave. It’s about being smart. I avoided penicillin for 15 years because my mom said I was allergic. Turns out I had a GI issue. Now I take it without a second thought. My insurance paid for the test. My doctor didn’t charge me extra. It took 20 minutes. And I saved myself from 15 years of weaker, costlier, riskier antibiotics. Do the math. Do the test. Your future self will high-five you.
Frank Dahlmeyer
December 2, 2025 AT 21:21THIS. I’ve spent the last 10 years working in rural clinics where people are terrified of antibiotics because of some childhood rash or a stomach ache from 1998. We’ve started running penicillin tests on-site now-15-minute results, $25 out-of-pocket, and 80% of people turn out to be fine. We’ve cut C. diff rates by nearly half. It’s not magic. It’s just asking the right questions. If your doctor doesn’t ask you about timing, symptoms, and severity-they’re not doing their job. Demand better. Your body deserves better than a label from 1992.