What Is Variceal Bleeding and Why It’s Life-Threatening
Variceal bleeding isn’t just a complication-it’s a medical emergency. It happens when swollen veins in the esophagus or stomach rupture, often without warning. These veins, called varices, form because of high pressure in the portal vein, the main blood vessel carrying blood from the intestines to the liver. When the liver is damaged by cirrhosis, it can’t handle the blood flow, so pressure builds up. Once that pressure hits 12 mmHg or more, the veins bulge and thin out until they burst.
Every year in the U.S., about 250,000 people experience variceal bleeding. About 1 in 5 of them die within six weeks. That’s why speed and precision matter. The goal isn’t just to stop the bleeding-it’s to stop it fast, prevent it from coming back, and treat the root cause: liver damage.
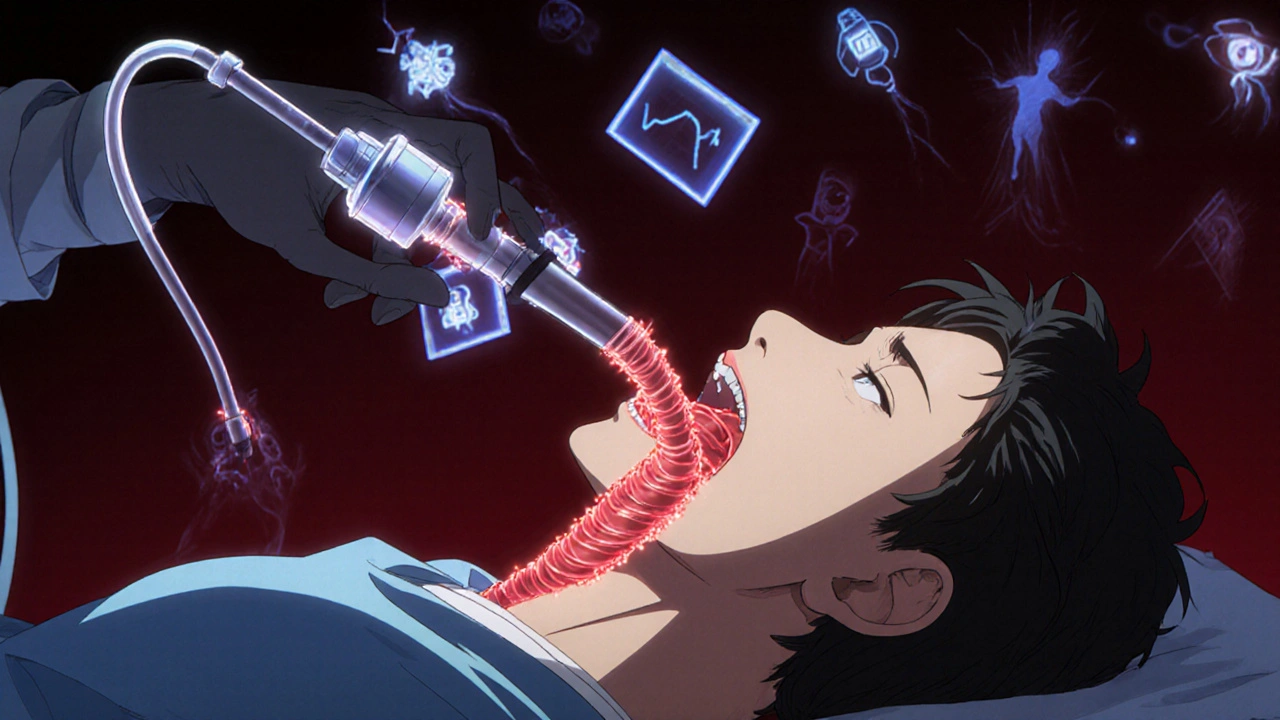
Endoscopic Band Ligation: The Gold Standard for Stopping Bleeding
If you’re bleeding from varices, the first thing doctors do is reach for an endoscope. Not a scalpel, not a drug-just a thin tube with a camera and a tiny rubber band launcher. This is endoscopic band ligation (EBL), and it’s the most effective way to stop active bleeding right now.
The procedure works by placing 6-8 tiny rubber bands around the swollen veins. The bands cut off blood flow, causing the varices to shrink and scar over. Success rates? Around 90-95% when done within 12 hours of bleeding starting. That’s the window doctors live by. Delay it, and the chance of rebleeding jumps.
Most patients need 3-4 sessions, spaced two weeks apart, to fully eliminate the varices. Each session costs between $1,200 and $1,800 in the U.S., and while it’s not fun-many report throat pain for weeks-it’s far safer than the old method, sclerotherapy, which caused scarring and strictures in 15% of cases. Modern multi-band devices like the Boston Scientific Six-Shot system cut procedure time by 35%, making it faster and more precise.
But banding isn’t perfect. If the bleeding is too heavy, the endoscopist can’t see clearly. In those cases, success drops to 85% or lower. That’s why it’s always paired with medication.
Beta-Blockers: The Silent Shield Against Rebleeding
Stopping the bleeding is only half the battle. Preventing it from coming back is where beta-blockers come in. These aren’t just heart meds-they’re lifesavers for people with cirrhosis.
Two drugs lead the pack: propranolol and carvedilol. Both lower the pressure in the portal vein by reducing heart output and blood flow to the liver. The target? Drop the hepatic venous pressure gradient (HVPG) to 12 mmHg or lower, or cut it by 20% from baseline. That’s the magic number that cuts rebleeding risk in half.
Carvedilol is now the preferred choice. In a 2021 trial of 287 patients, it lowered portal pressure by 22%, compared to 15% with propranolol. It’s more effective, and for many, easier to tolerate. But there’s a catch: carvedilol costs $25-$40 a month, while generic propranolol runs $4-$10. That price gap forces real choices for patients without good insurance.
Side effects are common. Fatigue, dizziness, low heart rate-about 1 in 3 people can’t handle the full dose. One Reddit user wrote, “Propranolol made me so tired I couldn’t get out of bed.” Others switched to carvedilol and found relief. But not everyone can use these drugs. If you have asthma, severe heart failure, or a very slow heartbeat, beta-blockers are off-limits.
Here’s the key point: beta-blockers alone won’t stop active bleeding. They’re for prevention. The 2022 AASLD guidelines say it clearly-never rely on them alone during a bleed. They’re the backup plan, not the first line.

When Banding and Beta-Blockers Aren’t Enough
Some patients still rebleed. That’s where things get more complex. If you’re high-risk-Child-Pugh B with active bleeding or Child-Pugh C-you might need something stronger: a TIPS procedure.
TIPS stands for transjugular intrahepatic portosystemic shunt. It’s a tiny metal tube placed inside the liver to create a new path for blood, bypassing the blocked areas. It’s not surgery, but it’s invasive. A radiologist threads a catheter through the neck vein into the liver to install the shunt. It works. In one landmark study, patients with TIPS had an 86% one-year survival rate compared to 61% with standard care.
But there’s a cost. About 30% of patients develop hepatic encephalopathy-confusion, memory loss, even coma-because toxins that the liver normally filters now bypass it. That’s why TIPS isn’t for everyone. Only 45% of U.S. hospitals have the trained teams to do it within 24 hours. Many patients wait too long, or never get it at all.
For gastric varices (bleeding in the stomach), banding often fails. In those cases, doctors turn to BRTO-balloon-occluded retrograde transvenous obliteration. A 2023 analysis of over 7,000 patients showed 30-day mortality was 6.2% with banding alone, but only 2.8% when combined with BRTO. That’s a big difference.
What Patients Really Experience
Behind the statistics are real people. On Reddit, one user said, “Banding stopped my bleeding immediately. I was out in three days.” Another wrote, “I dread the banding appointments every two weeks, but I know it’s saving my life.”
But the emotional toll is heavy. A 2022 survey by the American Liver Foundation found 42% of patients couldn’t tolerate beta-blockers because of fatigue. Others struggled with the cost. One person shared, “Carvedilol costs $35 a month copay. I skip doses to make it last.”
Even when treatment works, rebleeding happens. A 2023 report found 65% of patients had at least one more bleed within a year, even with perfect care. That’s why follow-up isn’t optional-it’s survival.

Prevention: The Most Important Step
The best way to avoid variceal bleeding is never to let it happen. That means screening. If you have cirrhosis, you should get an endoscopy every 1-2 years to check for varices. If they’re small, start beta-blockers. If they’re large, consider banding-even if you haven’t bled yet.
Primary prevention saves lives. Carvedilol is now being studied as a possible first-line option for people with large varices but no prior bleeding. Early data suggests it’s just as effective as banding, with fewer procedures and less risk.
But prevention isn’t just about drugs and devices. It’s about stopping liver damage before it starts. Cut alcohol. Manage hepatitis. Control diabetes. These aren’t suggestions-they’re the foundation of everything else.
What’s Next in Treatment
The future is coming fast. In 2023, the FDA approved a new long-acting form of octreotide-Sandostatin LAR-that only needs one monthly injection instead of daily shots. That could help patients who struggle with adherence.
AI is being tested to predict who’s most likely to bleed. Early models use liver scans, blood tests, and even voice patterns to spot risk before it turns into an emergency. If this works, we could shift from reactive to preventive care.
Another promising development? Percutaneous transsplenic TIPS. Right now, TIPS requires highly trained radiologists in big hospitals. This new method could be done by general interventionalists, making it available in 75% of U.S. hospitals by 2027-up from just 45% today.
But equity remains a problem. Uninsured patients die from variceal bleeding at 35% higher rates than those with insurance. Access to endoscopy, beta-blockers, and TIPS isn’t equal. That’s the real challenge ahead.
Final Takeaways
- Variceal bleeding is deadly, but treatable-if you act fast.
- Endoscopic banding is the fastest, most reliable way to stop active bleeding.
- Beta-blockers (especially carvedilol) cut rebleeding risk in half and should start right after bleeding stops.
- TIPS works for high-risk patients but brings risks like confusion and memory problems.
- Prevention through screening and early treatment saves more lives than emergency care.
- Cost, access, and side effects are real barriers. Talk to your care team about options.

Conor McNamara
November 18, 2025 AT 06:32Leilani O'Neill
November 18, 2025 AT 12:08Riohlo (Or Rio) Marie
November 18, 2025 AT 14:59steffi walsh
November 20, 2025 AT 10:38Louie Amour
November 20, 2025 AT 21:27Kristina Williams
November 22, 2025 AT 07:53Shilpi Tiwari
November 22, 2025 AT 10:38Christine Eslinger
November 24, 2025 AT 02:22Denny Sucipto
November 24, 2025 AT 16:25